- Review
- Open access
- Published:
A Review on Lower Limb Rehabilitation Exoskeleton Robots
Chinese Journal of Mechanical Engineering volume 32, Article number: 74 (2019)
Abstract
Lower limb rehabilitation exoskeleton robots integrate sensing, control, and other technologies and exhibit the characteristics of bionics, robotics, information and control science, medicine, and other interdisciplinary areas. In this review, the typical products and prototypes of lower limb exoskeleton rehabilitation robots are introduced and state-of-the-art techniques are analyzed and summarized. Because the goal of rehabilitation training is to recover patients’ sporting ability to the normal level, studying the human gait is the foundation of lower limb exoskeleton rehabilitation robot research. Therefore, this review critically evaluates research progress in human gait analysis and systematically summarizes developments in the mechanical design and control of lower limb rehabilitation exoskeleton robots. From the performance of typical prototypes, it can be deduced that these robots can be connected to human limbs as wearable forms; further, it is possible to control robot movement at each joint to simulate normal gait and drive the patient’s limb to realize robot-assisted rehabilitation training. Therefore human–robot integration is one of the most important research directions, and in this context, rigid-flexible-soft hybrid structure design, customized personalized gait generation, and multimodal information fusion are three key technologies.
1 Introduction
A rehabilitation robot, which is a robot directly serving humans, has extensive application prospects in rehabilitation therapy with high professional requirements. Therefore, it is of great importance to develop advanced rehabilitation robots.
Research on lower limb rehabilitation robots for patients with limb movement disorders is an important part of rehabilitation robot research. By 2030, 18.2% of China’s population will be over the age of 65. Due to an aging society and improving living standards, the number of people with limb dyskinesia is increasing rapidly. Limb movement disorders can lead to abnormal gait and affect normal walking. For patients with lower limb movement disorder, active rehabilitation training should be started as early as possible. In China, which has the highest stroke rate in the world [1], there are nearly 15 million disabled people with lower limb motor dysfunctions, such as cerebral palsy, hemiplegia, and paraplegia, and nearly 40 million disabled elderly people who have lost the ability to walk, due to aging. About 350,000 people are in urgent need of rehabilitation technical personnel, but less than 20,000 personnel are available. Therefore, lower limb rehabilitation robots are of great significance. The use of rehabilitation robots can reduce the burden on therapists, realize data detection during training, and aid the quantitative evaluation of recovery in a controllable and repeatable manner [2].
Lower limb rehabilitation exoskeleton robots, which are a major class of rehabilitation robots, connect with the human body in a wearable way and can control the movement of all joints in the training process. Research on lower limb rehabilitation exoskeleton robots began in the 1960s [3, 4]. Due to technical limitations, these early robots failed to reach the expected targets, but laid the foundation for follow-up studies. In recent decades, especially after Lokomat was applied in clinical rehabilitation, lower limb rehabilitation exoskeleton robots have gradually become a major research topic. They are mainly used to provide power assistance and rehabilitation to the elderly and patients with lower limb motor dysfunctions. Exoskeleton robot technology is a comprehensive technology that integrates sensing, control, information and computer science to provide a wearable mechanical device. Many enterprises and research institutions have carried out relevant research work and achieved several milestones in the theory and application of these robots. According to their application, these robots are divided into two types, namely for treadmill-based and overground applications. Patients can receive gait training from treadmill-based exoskeleton robots on a treadmill. In these robots, in addition to the exoskeleton that is used to provide assistance to leg movement [3], a body weight support (BWS) system is required to reduce gravitational forces acting on the legs, ensure safety, and maintain balance; some examples of such robots include ALEX [2], Lokomat [4], and LOPES [5], as shown in Figure 1. Overground exoskeleton robots help patients in regaining overground gait, as shown in Figure 2; examples include eLEGS (Exoskeleton Lower limb Gait System) [6, 7], Indego [8], ReWalk [9], MINDWALKER [10, 11], and HAL (Hybrid Assistive Limb) [12].
At present, a large gap exists in rehabilitation robot technology between China and the developed countries. China urgently requires rehabilitation-assistive devices and has the largest market potential in the world. By 2020, the industrial scale is expected to exceed 700 billion. Universities and institutes in China [13,14,15,16,17,18,19,20,21,22] have conducted a number of studies and achieved some promising results. However, deep disparities exist between Chinese and overseas research, and no systematic industry has yet been formed. Therefore, China’s lower limb rehabilitation exoskeleton robot research has the potential to produce another revolution in the robot industry.
Hence, in this paper, we present a review on lower limb rehabilitation exoskeleton robots. Research and results in mechanical design and control methods are discussed after collating a summary on human gait analysis. The state-of-the-art research on lower limb rehabilitation exoskeleton robots is described and human–robot integration, which is one of the most important research directions, is discussed.
2 Human Gait Analysis
Wearability is one of the most vital features of lower limb rehabilitation exoskeleton robots and hence such robots must have good human compatibility. Therefore, an illustration of lower limb anatomy and human gait analysis can provide the underlying basis for the design and control of lower limb exoskeleton rehabilitation robots.
2.1 Anatomy of Lower Limbs
The human walking process is mainly accomplished by lower limbs, and hence, analyzing their structure and movement characteristics is necessary.
Walking is achieved by coordination between the pelvis, hip, knee, and ankle. Their ranges of motion (ROM) are illustrated in Table 1. The pelvis is located between the trunk and thighs. As a ball-and-socket joint, the hip is formed by the head of the femur and pelvic bone and it allows simultaneous movement between the thighs and pelvis [23]. It allows sagittal flexion/extension, frontal abduction/adduction, and transverse external/internal rotation [24]. Knee is a joint complex containing tibiofemoral and patellofemoral joints. Their movement occurs in two planes, allowing sagittal flexion/extension and transverse internal/external rotation [23]. During walking, knees perform important functions. In the swing phase, knees shorten leg length by flexion [25]. In the stance phase, they remain flexed to absorb shock and transmit forces through legs. The ankle/foot is a complex structure that absorbs this shock and imparts thrust to the body. Ankle movements mainly occur about talocrural and subtalar joints [24]. The talocrural joint is located between the talus, distal tibia, and fibula to provide plantar/dorsiflexion as a hinge joint, in which the surface of one bone is spool-like and the surface of the other bone is concave. The subtalar joint is located between the calcaneus and talus and allows eversion/inversion and internal/external rotation. The basis for the mechanical design of rehabilitation exoskeleton robots is provided by an analysis of the lower limb structure.
2.2 Analysis on Human Gait
The normal gait pattern of patients cannot be measured directly because of their impaired motor functions. Therefore, it is necessary to conduct rehabilitation training and evaluate normal gait data, which is significant in clinical applications. Patients with hemiplegia or physical disabilities often follow a predetermined trajectory in their rehabilitation. These predetermined trajectories can be obtained from normal gait data collection. Through gait analysis, the relevant characteristics of human gait can be revealed. Step length, width, and speed are all used for human walking gait characterization. Thus, human body movement parameters and structural parameters have a significant influence on human gait characteristics.
Human gait is affected by walking speed [26, 27] as confirmed by an analysis of gait parameters [28] and joint angles [29], as confirmed by recording and analyze the gait data with different walking speeds on a walkway [30] or treadmill [31]. Because most rehabilitation robots use a body support system during rehabilitation training, analyzing human gait on a treadmill is necessary. Additionally, studies have revealed that body height, as a structural parameter, has limited effect on the human gait as compared to walking speed. This was proved by comparing the difference in the correlation between regression models when using speed and normalized speed (normalized to leg length) [30, 32] or by using step-wise regression in regression models by including body height [31] as a parameter. Further, these studies focused on the effect of these parameters on joint angles. Studies have also outlined the relationship between gait parameters and the body mass index (BMI) [26, 33]. These studies provide a foundation for control over lower limb rehabilitation exoskeleton robots.
3 Mechanics of Lower Limb Rehabilitation Exoskeleton Robots
Lower limb rehabilitation exoskeleton robots need a mechanical structure matching human lower limbs to realize force and energy transmission through the wearable connection. These can be achieved by designing the appropriate robot mechanism and actuation. An overview of the mechanics involved is presented in Table 2.
3.1 Anatomy of Human Upper Limbs
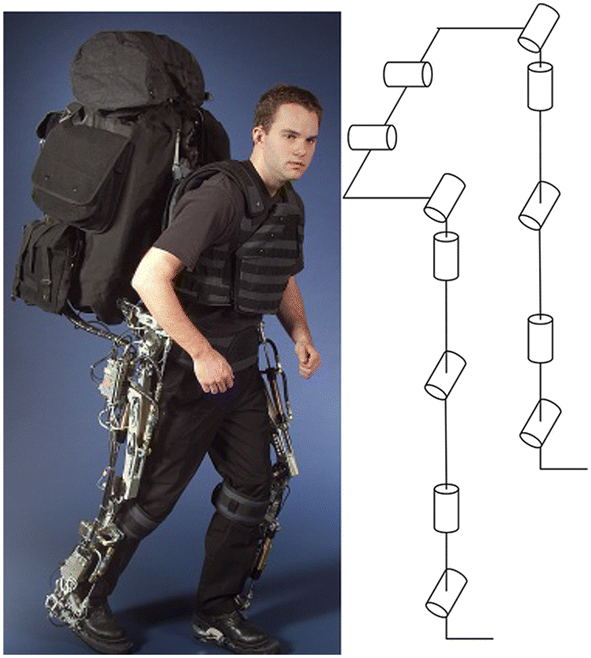
The mechanism of lower limb rehabilitation exoskeleton robots should realize movement matching with human lower limbs. The mechanism design of the Berkeley exoskeleton system (BLEEX) laid a foundation for subsequently developed robots. To ensure safety and avoid collisions maximally with users, BLEEX is almost anthropomorphic but does not include all the degrees of freedom available for human legs (Figure 3). Additionally, BLEEX joints are purely rotary joints and hence, are different from human joints [34]. The hip is simplified as three rotatory joints to achieve flexion/extension, abduction/extension, and internal/external rotation. The knee is simplified as a rotating joint to achieve pure sagittal rotation. The ankle is simplified into three rotation joints to achieve plantar/dorsiflexion, eversion/inversion and internal/external rotation. The configuration of the current lower limb exoskeleton robots, such as ALEX [35], Lokomat [4, 36], LOPES [37, 38], Rewalk [9], Rex [39] and HAL [40], is mainly based on BLEEX.
Biomechanical design of BLEEX [41]
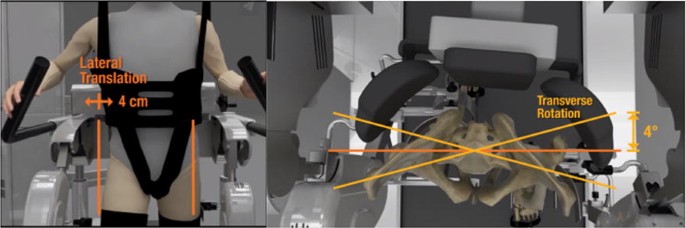
Due to the existence of the BWS system and the fact that the robot body is often connected to a fixed platform, an important feature of treadmill-based exoskeleton robots is that the patient does not need to carry the entire weight of the robot, which complicates the mechanical structure of the robot. At the same time, rehabilitation training on a treadmill requires less room, but there is a difference between gait on the treadmill and natural gait [42, 43], which is an important aspect in clinical evaluations [44,45,46,47]. Additional mechanisms were designed for pelvic movement. Pelvis motion is also being integrated into new robotic devices, such as KineAssist [48,49,50]. ALEX III can actively control motions of the pelvis [45, 51]. The new version of Lokomat includes an optional FreeD module to improve therapy by allowing for pelvic lateral translation and transverse rotation, as shown in Figure 4.
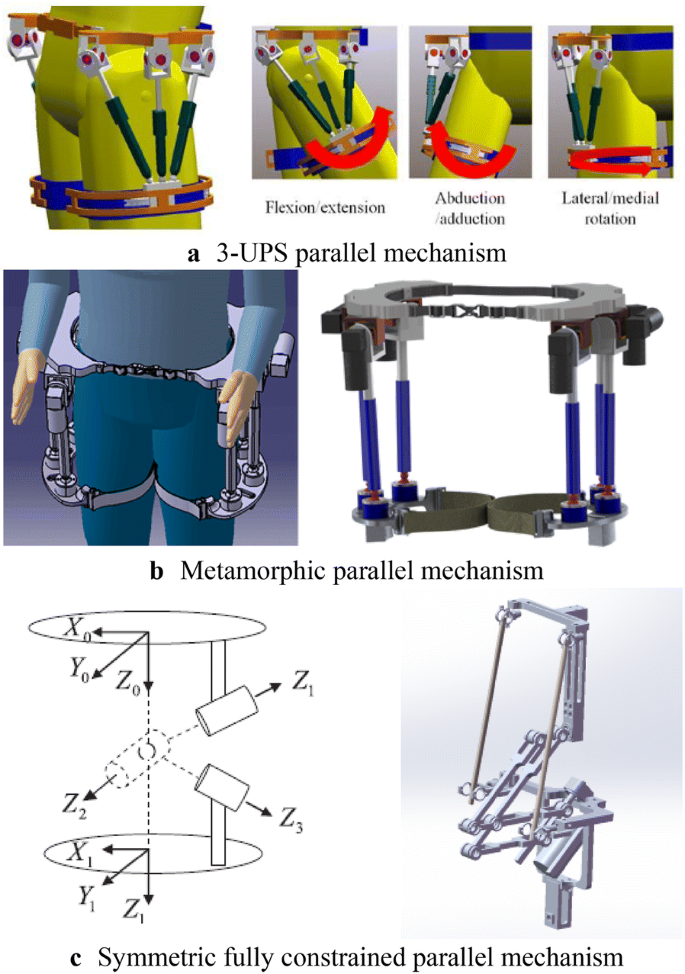
Such simplified design means that there is a motion mismatch between the robot and human, which is manifested in the mismatch between the joint centers of the robot and human. Designing an innovative mechanism can offer a solution to this problem. For hip joints, a parallel structure is adopted to realize three rotational motions and automatic centering with the human hip [52,53,54] as shown in Figure 5. When a 3-UPS parallel mechanism is mounted on the human waist and thigh, the thigh of the human and the mechanism are connected as a whole, which can be considered as a 3-UPS/1-S parallel mechanism [52] (Figure 5(a)). A novel metamorphic parallel mechanism was applied for lower limb rehabilitation using two configurations, 3-UPS/S and 2-RPS/UPS/S, by taking into account the human hip joint to satisfy different demands of patients at different phases of rehabilitation therapy [53] (Figure 5(b)). An asymmetric fully constrained parallel mechanism prototype is designed for hip joint assistance and rehabilitation and employs pantographs as three-rotation constrained legs instead of using three serial rotation joints-leg to avoid disadvantages such as singularity, uncertainty, or interference with other legs [54] (Figure 5(c)).
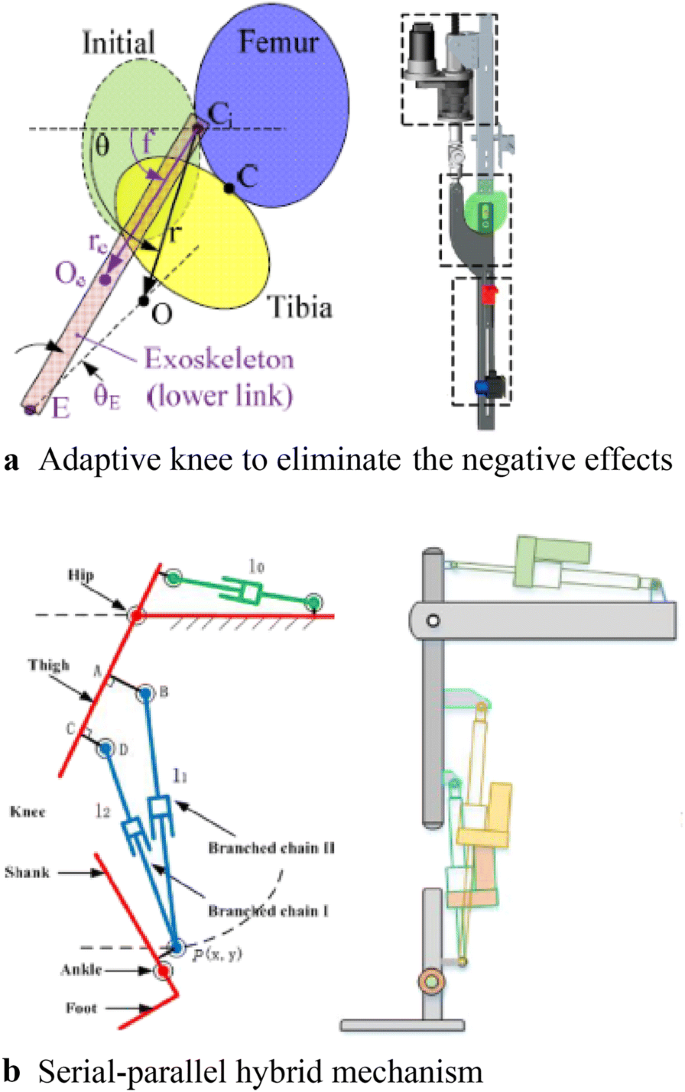
The knee joint is treated as a rotating joint in the simplification process and only the flexion and extension motion are considered. In fact, knee motion is relatively complex and hence different mechanisms have been designed to solve this problem, as shown in Figure 6. For the knee joint, an adaptive knee was used and it could effectively eliminate negative effects on human knees [55] (Figure 6(a)). Based on the knee joint complex, axial translational motion was coupled with rotational motion and a serial-parallel hybrid mechanism was designed for lower limb rehabilitation [17] (Figure 6(b)).
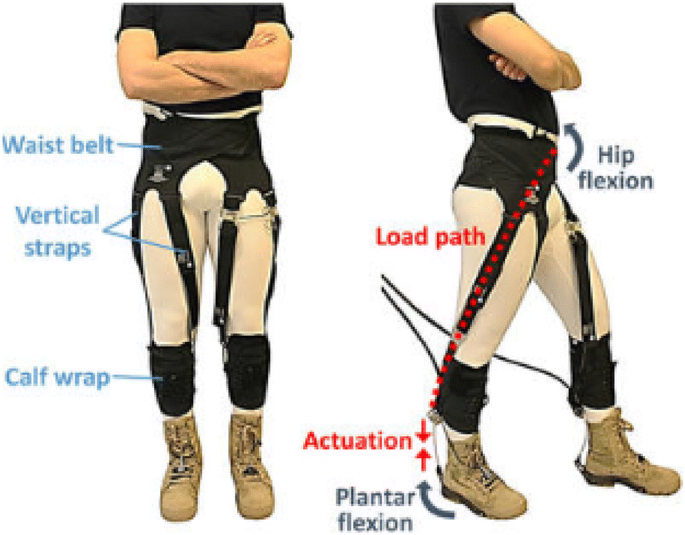
The human body is a coupled structure based on bone-muscle tissue structure and characteristics. According to this principle, some scholars have suggested a new kind of structure for lower limb rehabilitation robots. There is no rigid support for the mechanical structure but it includes a soft body and software structure using cables to provide power; this reduces response to muscle contractions and energy consumption of the body. This design for coupled wearable robots is expected to pave a new research direction [56] (Figure 7).
3.2 Actuation Design
Most lower limb exoskeleton rehabilitation robots are driven by electric motors. In eLEGS, only sagittal flexion/extension for the hip and knee are actuated using motors while the ankle remains passive [57]. The hip and knee of Lokomat are actuated by motors with linear ball screws [58].
A remarkable feature of the above method is that the driver is directly placed on the robot body, which increases its mass and complexity. Therefore, using cable-driven motors can reduce the mass of the exoskeleton robot itself, because the motor and driver are placed on the platform instead of directly on the exoskeleton [59].
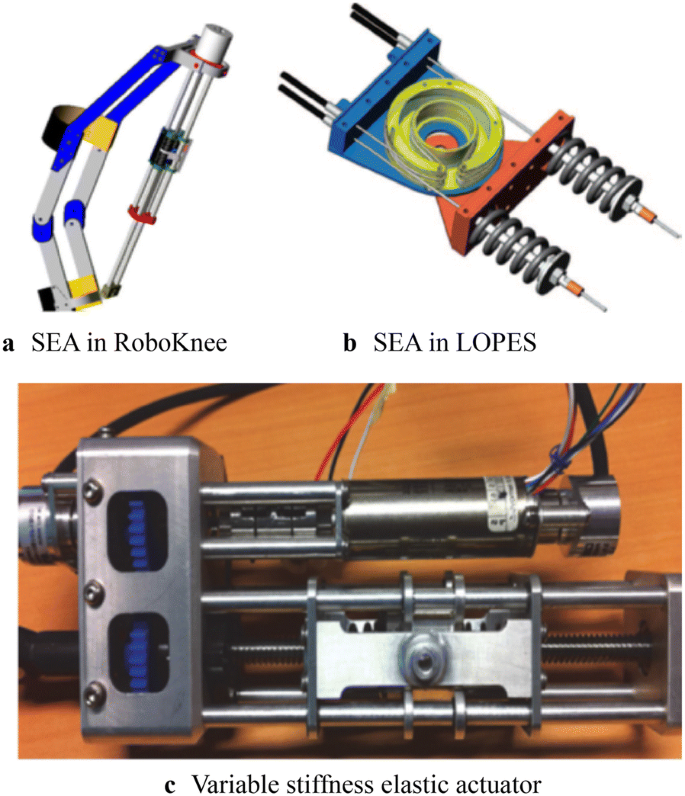
Lower limb rehabilitation exoskeletons are mainly driven by rigid transmission without compliance. This causes a large vibration impact, difficulty in directly controlling the force, and leads to a complicated robot system. Therefore, a series elastic drive (SEA) was designed to achieve force control and enhance drive flexibility in RoboKnee [60] (Figure 8(a)). SEA with a combination of cable-driven actuation was applied in LOPES [59] (Figure 8(b)). A variable stiffness elastic actuator was designed for lower limb exoskeletons by adjusting the stiffness of the elastic elements driven by series elasticity [61] (Figure 8(b)).
4 Control of Lower Limb Rehabilitation Robots
4.1 Trajectory Planning
The main purpose of rehabilitation training is to restore the lower limb motor functions of disabled patients to normal levels [62]; therefore, in the process of rehabilitation training, a normal gait pattern is required as a reference input to the control system, as a training goal, and as a rehabilitation evaluation standard. For patients with hemiplegia or physical disabilities, a predetermined trajectory is often used. These predetermined trajectories can be obtained from data on normal gait. However, due to the limited amount of data, it is difficult to match the obtained motion data with different human motion characteristics, and hence, a parameterized motion pattern generation method was proposed to predict data not present in the test sample.
The trajectories of Lokomat can be adjusted to a specific patient and step length [58]. In LOPES, trajectories are generated by a method based on regression analysis to reconstruct the body height and speed-dependent trajectories [31]; further, “complementary limb motion estimation” may be used to generate reference motion using the motion of healthy limbs [63]. When the collected number of samples is large enough, statistical learning techniques, such as the radial basis function neural networks (RBFs) [64] and multi-layer perceptron neural network (MLPNN) [65], are often used for motion prediction.
There is another type of gait planning that does not rely on specific data; however, it depends on the given gait parameters, such as step length and swing duration to generate gait patterns. The model predictive control (MPC) is used for online trajectory generation based on gait parameters [66].
4.2 Control System
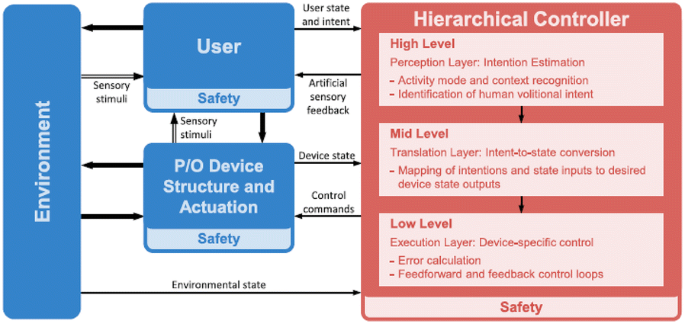
A hierarchical control strategy is used in most lower limb rehabilitation exoskeleton robots. Generally, the control system is divided into two levels. The upper level is the decision-making layer, which realizes control decisions and trajectory generation, and the lower level is the servo layer, which realizes servo control of the drive system [65]. As for overground rehabilitation exoskeletons, they are divided into three layers due to the large number of movements involved (Figure 9). In particular, a human–robot interaction layer is added to adapt to the training needs of a variety of movements [6]. An overview of the control method of lower limb exoskeletons is shown in Table 3.
Generalized control framework for lower limbs [67]
In early rehabilitation stages, the lower limbs of patients are dragged for continuous passive motion (CPM) for passive training, which can effectively keep joints flexible for a long time. Correspondingly, position control ensures that the robot can accurately follow the desired position. In this case, movement information of the robot is measured by sensors, such as linear and rotary potentiometers [40, 68, 69], inertia measurement units (IMUs) [70, 71], torque sensors to measure torque [70, 71], and foot pressure sensors to measure the ground reaction to detect gait events [72, 73]. Control methods widely used in servo control have also been used in lower limb rehabilitation exoskeleton robots. For example, proportional derivative control (PD control) [68], computed torque control [74], fuzzy control [74], robust variable structure control [75], fuzzy proportional integral derivative control (PID contro), and sliding mode variable structure control [76] have been used for lower limb exoskeleton robots. Such position control is actually a type of tracking control. Force-position hybrid control was also used to adjust the output force exerted on the patient. This was the first impedance or admittance control strategy ever developed. It has been applied in the Lokomat to guide patients’ legs and supply hip and knee joint torque [4]. In LOPES, the robotic support was controlled using a virtual model controller (VMC) [69, 77].
All the control systems described above are passive in nature because the wearer is not considered in the system. By increasing active participation, the dependence of patients on robot assistance can be reduced by improving the effect of rehabilitation training. To achieve this effect, it is important to integrate people into the control system. As mentioned earlier, sensors have been used to measure human movement information and human–robot interaction information to control a robot. In ALEX a force field control is used to guide patients’ legs [45, 70].
Another way is to measure human biological signals such as electromyography (EMG) and electroencephalogram (EEG) signals, to perceive body movement. Currently, EMG signals are being used in robots such as HAL [78]. The EMG signal to be detected is used as a trigger switch to judge the timing of assistance provided by the robot [78, 79]. As continuous control, a proportional myoelectric control is used in the robotic ankle exoskeleton [80, 81]. However, EMG-based robot-assisted rehabilitation is only suitable for patients who are able to produce a sufficiently high level of muscle activity. Brain-machine interfaces to restore mobility in severely paralyzed patients [82] have been applied in many lower limb rehabilitation exoskeletons [39, 83,84,85]. However, this research is still in the early stages. All the systems described above rely on the presence of sensors and control the signals measured by sensors. Recently, robots not based on sensors have been developed. In this case, an admittance shaping controller is used [86].
5 Conclusions and Outlook
5.1 Conclusions
Lower limb rehabilitation exoskeleton robots integrate sensing, control, and other technologies and exhibit characteristics of bionics, robotics, information and control science, medicine, and other interdisciplinary fields and therefore, have become a major research hotspot. In recent years, remarkable progress has been achieved in mechanical design and control system design, based on which, several products have been commercialized. However, there is still a large research gap with respect to human–robot integration. The wearer (patient) should organically combine with the robot to form a whole. Only when true integration of the human body and robot is realized can rehabilitation training be truly effective.
5.2 Outlook
The problem of human–robot integration is a current research hot spot. The National Natural Science Foundation of China (NSFC) has launched the Tri-Co Robot (i.e., the Coexisting-Cooperative-Cognitive Robot), a major research program in 2017, with research themes of robot structure design and control, multi-mode dynamic perception, and natural interaction [87]. Human–robot integration is a key issue in the design and control of lower limb rehabilitation exoskeleton robots. In summary, such integration should include three components, namely structure, movement, and response.
Humanoid structures and flexible drive systems should be designed to achieve structural integration between robots and patients. Currently, a simplified human movement model and a rigid structural design are adopted, causing movement mismatch between a robot and human and affecting wearability and rehabilitation training. Therefore, SEA is being used to increase the flexibility of the local structure. The addition of flexibility inevitably leads to structural complexity and difficulty in control. An ideal robot structure is a rigid-flexible-soft hybrid structure. However, rigid-soft-soft coupling configurations should be designed to effectively transfer energy from a robot to a human. At the same time, modular designs for exoskeleton mechanism should be explored. In fact, many active orthosis devices can also be referred to as modular single-joint exoskeletons.
Customized and personalized gait patterns should be generated to achieve motion integration between robots and patients. A normal movement mode is often required as a reference and input to the control system as the expected robot movement, training target, and evaluation standard. For patients with hemiplegia or other physical disabilities, a predetermined trajectory is often used in rehabilitation. These predetermined trajectories can be obtained from normal gait data collection. However, due to the limited amount of data collected, it is difficult for the obtained motion data to match different motion characteristics of the human body, and hence, a parameterized motion pattern generation method has been proposed. However, the current planning and gait generation methods based on the biped robot control theory and human natural gait cannot achieve a perfect match; gait generation is mainly focused on the sagittal plane and does not account for human three-dimensional gait characteristics. The mechanism of how human gait is affected by motion and structural parameters is not yet fully understood, and hence, it is difficult to realize a perfect integration of motion levels.
Multimodal information fusion should be used to achieve motion integration between humans and machines. Current research on the design of sensing systems indicates that it is not enough to measure a robot’s movement information; instead, people also should be included in the system, not only to measure human body movement information and biological signals but also to collect interaction information between a human and the force exerted by the robot. However, it can be imagined that more information is not always better as redundant information increases the complexity of a system and affects its practical application. In the process of rehabilitation training, lower limb rehabilitation exoskeleton robots need to participate in effective dynamic interaction with the patient. Such rehabilitation training can effectively improve the level of active participation of the patient and significantly enhance the rehabilitation effect. However, the evaluation method of the robot itself lacks a set of system indicators for the adaptability and degree of matching with the human body. Hence, it is necessary to study multimodal information to realize effective human–robot integration.
References
G L R O Collaborators. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. New England Journal of Medicine, 2018, 379(25): 2429-2437.
S K Banala, S H Kim, S K Agrawal, et al. Robot assisted gait training with active leg exoskeleton (ALEX). IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2009, 17(1): 2-8.
G Chen, C K Chan, Z Guo, et al. A review of lower extremity assistive robotic exoskeletons in rehabilitation therapy. Critical Reviews in Biomedical Engineering, 2013, 41(4-5): https://doi.org/10.1615/critrevbiomedeng.2014010453.
M Bernhardt, M Frey, G Colombo, et al. Hybrid force-position control yields cooperative behaviour of the rehabilitation robot LOKOMAT. International Conference on Rehabilitation Robotics, 2005: 536-539.
Van Asseldonk E H, Van Der Kooij H. Robot-aided gait training with LOPES. Neurorehabilitation Technology, Springer, 2012.
S T Alan. Control and trajectory generation of a wearable mobility exoskeleton for spinal cord injury patients. University of California, Berkeley, 2011.
S K Ann. Development of a human machine interface for a wearable exoskeleton for users with spinal. University of California, Berkeley, 2011.
R J Farris, H A Quintero, M Goldfarb. Preliminary evaluation of a powered lower limb orthosis to aid walking in paraplegic individuals. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2011, 19(6): 652-659.
G Zeilig, H Weingarden, M Zwecker, et al. Safety and tolerance of the ReWalk™ exoskeleton suit for ambulation by people with complete spinal cord injury: A pilot study. The Journal of Spinal Cord Medicine, 2012, 35(2): 96-101.
J Gancet, M Ilzkovitz, E Motard, et al. MINDWALKER: going one step further with assistive lower limbs exoskeleton for SCI condition subjects. IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, Rome, Italy, June 24-27, 2012: 1794-1800.
J Gancet, M Ilzkovitz, G Cheron, et al. MINDWALKER: a brain controlled lower limbs exoskeleton for rehabilitation. Potential applications to space. 11th Symposium on Advanced Space Technologies in Robotics and Automation, Noordwijk, Netherlands, April 12-15, 2011: 12-14.
H Satoh, T Kawabata, Y Sankai. Bathing care assistance with robot suit HAL. IEEE International Conference on Robotics and Biomimetics, Guilin, China, December 18-22, 2009: 498-503.
H Yan, C Yang. Design and validation of a lower limb exoskeleton employing the recumbent cycling modality for post-stroke rehabilitation. Proceedings of the Institution of Mechanical Engineers, Part C: Journal of Mechanical Engineering Science, 2014, 228(18): 3517-3525.
Y Miao, F Gao, P Dan. Mechanical design of a hybrid leg exoskeleton to augment load-carrying for walking. International Journal of Advanced Robotic Systems, 2013, 10: https://doi.org/10.5772/57238.
P Pei, Z Pei, Z Shi, et al. Sensorless control for joint drive unit of lower extremity exoskeleton with cascade feedback observer. Mathematical Problems in Engineering, 2018, 3029514: 1-11, https://doi.org/10.1155/2018/3029514.
D Liu, Z Tang, Z Pei. Variable structure compensation PID control of asymmetrical hydraulic cylinder trajectory tracking. Mathematical Problems in Engineering, 2015, 890704: 1-9. https://doi.org/10.1155/2015/890704.
M Lyu, W Chen, X Ding, et al. Design of a biologically inspired lower limb exoskeleton for human gait rehabilitation. Review of Scientific Instruments, 2016, 87(10): 104301.
R Huang, H Cheng, H Guo, et al. Hierarchical learning control with physical human-exoskeleton interaction. Information Sciences, 2018, 432: 584-595.
R Huang, H Cheng, Y Chen, et al. Optimisation of reference gait trajectory of a lower limb exoskeleton. International Journal of Social Robotics, 2016, 8(2): 223-235.
D Wang, K Lee, J Ji. A passive gait-based weight-support lower extremity exoskeleton with compliant joints. IEEE Transactions on Robotics, 2016, 32(4): 933-942.
X Wu, D Liu, M Liu, et al. Individualized gait pattern generation for sharing lower limb exoskeleton robot. IEEE Transactions on Automation Science and Engineering, 2018, 15(4): 1459-1470.
C Chen, X Wu, D Liu, et al. Design and voluntary motion intention estimation of a novel wearable full-body flexible exoskeleton robot. Mobile Information Systems, 2017: https://doi.org/10.1155/2017/8682168.
D A Neumann. Kinesiology of the musculoskeletal system: foundations for rehabilitation. Elsevier Health Sciences, 2013.
J E Muscolino. Kinesiology: The skeletal system and muscle function. Elsevier Medicine, 2011.
A D Kuo. The six determinants of gait and the inverted pendulum analogy: A dynamic walking perspective. Human Movement Science, 2007, 26(4): 617-656.
E F Chehab, T P Andriacchi, J Favre. Speed, age, sex, and body mass index provide a rigorous basis for comparing the kinematic and kinetic profiles of the lower extremity during walking. Journal of Biomechanics, 2017, 58: 11-20.
J W Kwon, S M Son, N K Lee. Changes of kinematic parameters of lower extremities with gait speed: a 3D motion analysis study. Journal of Physical Therapy Science, 2015, 27(2): 477-479.
S Al-Obaidi, J C Wall, A Al-Yaqoub, et al. Basic gait parameters: A comparison of reference data for normal subjects 20 to 29 years of age from Kuwait and Scandinavia. Journal of Rehabilitation Research and Development, 2003, 40(4): 361-366.
T J Cunningham. Three-dimensional quantitative analysis of the trajectory of the foot while running. University of Kentucky, 2007.
J L Lelas, G J Merriman, P O Riley, et al. Predicting peak kinematic and kinetic parameters from gait speed. Gait & Posture, 2003, 17(2): 106-112.
B Koopman, E Van Asseldonk, H Van der Kooij. Speed-dependent reference joint trajectory generation for robotic gait support. Journal of Biomechanics, 2014, 47(6): 1447-1458.
M Hanlon, R Anderson. Prediction methods to account for the effect of gait speed on lower limb angular kinematics. Gait & Posture, 2006, 24(3): 280-287.
S Ko, S Stenholm, L Ferrucci. Characteristic gait patterns in older adults with obesity - results from the baltimore longitudinal study of aging. Journal of Biomechanics, 2010, 43(6): 1104-1110.
A B Zoss, H Kazerooni, et al. Biomechanical design of the Berkeley lower extremity exoskeleton (BLEEX). IEEE/ASME Transactions on Mechatronics, 2006, 1(2): 128-138.
S K Banala, S K Agrawal, S H Kim, et al. Novel gait adaptation and neuromotor training results using an active leg exoskeleton. Mechatronics, 2010, 15(2): 216-225.
R Riener, L Lunenburger, S Jezernik, et al. Patient-cooperative strategies for robot-aided treadmill training: first experimental results. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2005, 13(3): 380-394.
J Meuleman, E Van Asseldonk, G Van Oort, et al. LOPES II—design and evaluation of an admittance controlled gait training robot with shadow-leg approach. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2016, 24(3): 352-363.
R Ekkelenkamp, J Veneman, H Van der Kooij. LOPES: Selective control of gait functions during the gait rehabilitation of CVA patients. International Conference on Rehabilitation Robotics, Chicago, IL, USA, June 28 - July 1, 2005: 361-364.
N Kwak, K Muller, S Lee. Toward exoskeleton control based on steady state visual evoked potentials. International Winter Workshop on Brain-Computer Interface (BCI), Gangwon Province, Korea (South), February 17-19, 2014: 1-2.
A Tsukahara, Y Hasegawa, K Eguchi, et al. Restoration of gait for spinal cord injury patients using hal with intention estimator for preferable swing speed. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2015, 23(2): 308-318.
M W Whittle. Gait analysis: an introduction. Butterworth-Heinemann, 2014.
J H Hollman, M K Watkins, A C Imhoff, et al. A comparison of variability in spatiotemporal gait parameters between treadmill and overground walking conditions. Gait & Posture, 2016, 43: 204-209.
S J Lee, J Hidler. Biomechanics of overground vs. treadmill walking in healthy individuals. Journal of Applied Physiology, 2008, 104(3): 747-755.
J Mehrholz, L A Harvey, S Thomas, et al. Is body-weight-supported treadmill training or robotic-assisted gait training superior to overground gait training and other forms of physiotherapy in people with spinal cord injury? A systematic review. Spinal Cord, 2017, 55(8): 722-729.
S Srivastava, P Kao, S H Kim, et al. Assist-as-needed robot-aided gait training improves walking function in individuals following stroke. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2015, 23(6): 956-963.
T Senthilvelkumar, H Magimairaj, J Fletcher, et al. Comparison of body weight-supported treadmill training versus body weight-supported overground training in people with incomplete tetraplegia: a pilot randomized trial. Clinical Rehabilitation, 2015, 29(1): 42-49.
M Alcobendasmaestro, A Esclarínruz, R M Casadolópez, et al. Lokomat robotic-assisted versus overground training within 3 to 6 months of incomplete spinal cord lesion: randomized controlled trial. Neurorehabilitation & Neural Repair, 2012, 26(9): 1058.
S A Graham, C P Hurt, D A Brown. Minimizing postural demands of walking while still emphasizing locomotor force generation for nonimpaired individuals. IEEE Transactions on Neural Systems and Rehabilitation Engineering: A Publication of the IEEE Engineering in Medicine and Biology Society, 2018, 26(5): 1003-1010.
V C Dionisio, C P Hurt, D A Brown. Effect of forward-directed aiding force on gait mechanics in healthy young adults while walking faster. Gait & Posture, 2018, 64: 12-17.
J Patton, D A Brown, M Peshkin, et al. KineAssist: design and development of a robotic overground gait and balance therapy device. Topics in Stroke Rehabilitation, 2008, 15(2): 131-139.
D Zanotto, P Stegall, S K Agrawal. ALEX III: A novel robotic platform with 12 DOFs for human gait training. IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 2013, 2013: 3914-3919.
Y Yu, W Liang. Manipulability inclusive principle for hip joint assistive mechanism design optimization. The International Journal of Advanced Manufacturing Technology, 2014, 70(5-8): 929-945.
W Zhang, S Zhang, M Ceccarelli, et al. Design and kinematic analysis of a novel metamorphic mechanism for lower limb rehabilitation. Springer, Cham, 2016.
W Zhang, W Zhang, D Shi, et al. Design of hip joint assistant asymmetric parallel mechanism and optimization of singularity-free workspace. Mechanism and Machine Theory, 2018, 122: 389-403.
D Wang, K Lee, J Guo, et al. Adaptive knee joint exoskeleton based on biological geometries. IEEE/ASME Transactions on Mechatronics, 2014, 19(4): 1268-1278.
B T Quinlivan, S Lee, P Malcolm, et al. Assistance magnitude versus metabolic cost reductions for a tethered multiarticular soft exosuit. Science Robotics, 2017, 2(2): 1-10.
S A Kolakowsky-Hayner, J Crew, S Moran, et al. Safety and feasibility of using the EksoTM bionic exoskeleton to aid ambulation after spinal cord injury. Journal of Spine, 2013, 4: 1-8.
J Hidler, W Wisman, N Neckel. Kinematic trajectories while walking within the Lokomat robotic gait-orthosis. Clinical Biomechanics, 2008, 23(10): 1251-1259.
H Vallery, J Veneman, E Van Asseldonk, et al. Compliant actuation of rehabilitation robots. IEEE Robotics & Automation Magazine, 2008, 15(3): 60-69.
J E Pratt, B T Krupp, C J Morse, et al. The RoboKnee: an exoskeleton for enhancing strength and endurance during walking. Proceedings of IEEE International Conference on Robotics and Automation, New Orleans, LA, USA, April 26 - May 1, 2004: 2430-2435.
H Yu, S Huang, G Chen, et al. Human–robot interaction control of rehabilitation robots with series elastic actuators. Robotics, IEEE Transactions on., 2015, 31(5): 1089-1100.
E Sariyildiz, G Chen, H Yu. An acceleration-based robust motion controller design for a novel series elastic actuator. IEEE Transactions on Industrial Electronics, 2016, 63(3): 1900-1910.
H Vallery, R Burgkart, C Hartmann, et al. Complementary limb motion estimation for the control of active knee prostheses. Biomedizinische Technik/Biomedical Engineering, 2011, 56(1): 45-51.
K Seo, Y Park, S Yun, et al. Gait pattern generation for robotic gait rehabilitation system on treadmill. 14th International Conference on Control, Automation and Systems, KINTEX, Gyeonggi-do, Korea, October 22-25, 2014: 1090-1094.
H B Lim, T P Luu, K H Hoon, et al. Natural gait parameters prediction for gait rehabilitation via artificial neural network. IEEE/RSJ International Conference on Intelligent Robots and Systems, Taipei, Taiwan, China, October 18-22, 2010: 5398-5403.
L Wang, E H van Asseldonk, H van der Kooij. Model predictive control-based gait pattern generation for wearable exoskeletons. IEEE International Conference on Rehabilitation Robotics, ETH Zurich Science City, Switzerland, June 29 - July 1, 2011: 1-6.
M R Tucker, J Olivier, A Pagel, et al. Control strategies for active lower extremity prosthetics and orthotics: a review. Journal of Neuroengineering and Rehabilitation, 2015, 12(1): 1-30.
S Maggioni, L Lünenburger, R Riener, et al. Robot-aided assessment of walking function based on an adaptive algorithm. IEEE International Conference on Rehabilitation Robotics, Singapore, Aug. 11-14, 2015: 804-809.
B Koopman, E H van Asseldonk, H van der Kooij. Selective control of gait subtasks in robotic gait training: foot clearance support in stroke survivors with a powered exoskeleton. Journal of Neuroengineering and Rehabilitation, 2013, 10(3): 1-21.
X Jin, X Cui, S K Agrawal. Design of a cable-driven active leg exoskeleton (C-alex) and gait training experiments with human subjects. IEEE International Conference on Robotics and Automation, Seattle, Washington, USA, May 26-30, 2015: 5578-5583.
O Harib, A Hereid, A Agrawal, et al. Feedback control of an exoskeleton for paraplegics: toward robustly stable hands-free dynamic walking. IEEE Control Systems Magazine, 2018, 38(6): 61-87.
T Lenzi, M C Carrozza, S K Agrawal. Powered hip exoskeletons can reduce the user’s hip and ankle muscle activations during walking. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 2013, 21(6): 938-948.
D B Fineberg, P Asselin, N Y Harel, et al. Vertical ground reaction force-based analysis of powered exoskeleton-assisted walking in persons with motor-complete paraplegia. The Journal of Spinal Cord Medicine, 2013, 36(4): 313-321.
P K Jamwal, S Q Xie, S Hussain, et al. An adaptive wearable parallel robot for the treatment of ankle injuries. IEEE/ASME Transactions on Mechatronics, 2014, 19(1): 64-75.
S Hussain, S Q Xie, P K Jamwal. Robust nonlinear control of an intrinsically compliant robotic gait training orthosis. IEEE Transactions on Systems, Man, and Cybernetics: Systems, 2013, 43(3): 655-665.
Z Tang, D Shi, D Liu, et al. Electro-hydraulic servo system for Human Lower-limb Exoskeleton based on sliding mode variable structure control. Information and Automation (ICIA), 2013 IEEE International Conference on, 2013: 559-563.
J Pratt, C Chew, A Torres, et al. Virtual model control: An intuitive approach for bipedal locomotion. The International Journal of Robotics Research, 2001, 20(2): 129-143.
T Lenzi, S M De Rossi, N Vitiello, et al. Intention-based EMG control for powered exoskeletons. IEEE Trans. Biomed Eng., 2012, 59(8): 2180-2190.
H He, K Kiguchi. A study on EMG-based control of exoskeleton robots for human lower-limb motion assist. Information Technology Applications in Biomedicine, 2007. ITAB 2007. 6th International Special Topic Conference on, 2007: 292-295.
P Kao, C L Lewis, D P Ferris. Invariant ankle moment patterns when walking with and without a robotic ankle exoskeleton. Journal of Biomechanics, 2010, 43(2): 203-209.
D P Ferris, K E Gordon, G S Sawicki, et al. An improved powered ankle–foot orthosis using proportional myoelectric control. Gait & Posture, 2006, 23(4): 425-428.
A R Donati, S Shokur, E Morya, et al. Long-term training with a brain-machine interface-based gait protocol induces partial neurological recovery in paraplegic patients. Scientific Reports, 2016, 6: 30383.
D Liu, W Chen, Z Pei, et al. A brain-controlled lower-limb exoskeleton for human gait training. Review of Scientific Instruments, 2017, 88(10): 104302.
N Kwak, K Müller, S Lee. A lower limb exoskeleton control system based on steady state visual evoked potentials. Journal of Neural Engineering, 2015, 12(5): 56009.
R Xu, N Jiang, N Mrachacz-Kersting, et al. A closed-loop brain-computer interface triggering an active ankle-foot orthosis for inducing cortical neural plasticity. IEEE Transactions on Biomedical Engineering, 2014, 61(7): 2092-2101.
G Aguirre-Ollinger, U Nagarajan, A Goswami. An admittance shaping controller for exoskeleton assistance of the lower extremities. Autonomous Robots, 2016, 40(4): 701-728.
H Ding, X Yang, N Zheng, et al. Tri-Co Robot: a Chinese robotic research initiative for enhanced robot interaction capabilities. National Science Review, 2017, 5(6): 799-801.
Authors’ Contributions
XD was in charge of the whole trial; DS wrote the manuscript; WXZ and WZ assisted with structure and language of the manuscript. All authors read and approved the final manuscript.
Authors’ Information
Di Shi, born in 1988, is currently a PhD candidate at Robotics Institute, Beihang University, China. He received his bachelor degree from Wuhan University of Technology, China, in 2011. And he received his master degree from Beihang University, China, in 2014. His research interests include wearable lower limb rehabilitation robot control.
Wuxiang Zhang, born in 1978, is currently an associate professor at School of Mechanical Engineering and Automation, Beihang University, China. He received his PhD degree from Beihang University, China, in 2009. His research interests include the dynamics of compliant mechanical systems and robots, intelligent device and detection technology.
Wei Zhang, born in 1986, is currently a PhD candidate at Robotics Institute, Beihang University, China. He received his bachelor’s degree from Northwestern Polytechnical University, China, in 2009. His research interests include mechanical design of the wearable robot.
Xilun Ding, born in 1967, is currently a professor and a PhD candidate supervisor at School of Mechanical Engineering and Automation, Beihang University, China. He received his PhD degree from Harbin Institute of Technology, China, in 1997. His research interests include the dynamics of compliant mechanical systems and robots, nonholonomic control of space robots, dynamics and control of aerial robots, and biomimetic robots.
Acknowledgements
The authors sincerely thank Mr. Chong Qi, and Yixin Shao of Beihang University for their critical discussion and reading during manuscript preparation.
Competing Interests
The authors declare that they have no competing interests.
Funding
Supported by National Key R&D Program of China (Grant No. 2016YFE0105000) and National Natural Science Foundation of China (Grant No. 91848104).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shi, D., Zhang, W., Zhang, W. et al. A Review on Lower Limb Rehabilitation Exoskeleton Robots. Chin. J. Mech. Eng. 32, 74 (2019). https://doi.org/10.1186/s10033-019-0389-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10033-019-0389-8